Understanding Radiation Therapy for Kidney Cancer
- 657 Views
- Apollo Hospital Mumbai
- December 14, 2023
- Oncology
Verified by Dr. Sandeep De, Sr. Consultant Radiation Oncology, Apollo Cancer Centres, Navi Mumbai.
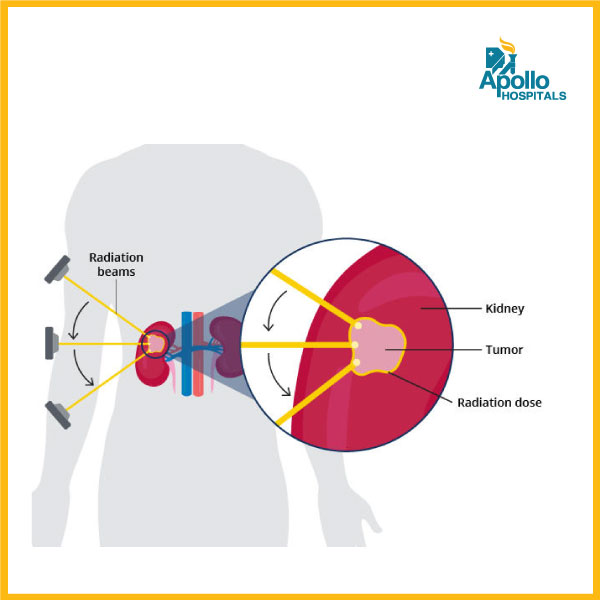
While surgery is often the primary treatment for kidney cancer, radiation therapy can play a crucial role in managing the disease. This specialized medical intervention uses high-energy rays or particles to destroy cancer cells and shrink tumors. Let’s delve into the details of radiation therapy in the context of kidney cancer.
The role of radiation therapy in kidney cancers, specifically renal cell carcinoma (RCC), has historically been limited due to the relative radio resistance of kidney tissues. However, there are certain scenarios where radiation therapy can be beneficial.
- Adjuvant Radiation Therapy
– Adjuvant radiation therapy is not a standard treatment for localized renal cell carcinoma after surgery. The primary treatment is surgical resection. However, in cases with positive surgical margins or certain high-risk features, adjuvant radiation therapy may be considered. The evidence supporting routine use is limited, and decisions are often made on a case-by-case basis (Kutikov et al., 2017).
2. Palliative Radiation Therapy
– Palliative radiation therapy plays a role in managing symptoms of advanced kidney cancer, especially when the disease has metastasized to bones or other sites. It can be effective in relieving pain, controlling bleeding, and stabilizing or preventing fractures in metastatic lesions.
3. Combination Therapy
– Studies exploring the combination of radiation therapy with systemic therapies, such as immunotherapy or targeted therapies, are ongoing. Combining these modalities may enhance treatment responses, particularly in cases where metastatic lesions are present.
4. Metastatic Disease
– In cases of oligometastatic disease (limited number of metastases), stereotactic body radiation therapy (SBRT) or focused radiation to specific metastatic sites may be considered. This approach aims to control metastatic lesions and potentially prolong progression-free survival.
5. Local Control in Unresectable Tumors
– For unresectable primary kidney tumors in certain cases, radiation therapy may be used to achieve local control. This is often considered when surgery is not a viable option due to the size or location of the tumor.
6. Stereotactic Body Radiotherapy (SBRT)
For patients with unresectable primary kidney tumors, especially in situations where surgery is not feasible or poses significant risks, SBRT may be considered. This approach enables the delivery of high doses of radiation to the tumor while minimizing exposure to surrounding healthy tissues. Studies have reported high local control rates with SBRT for both primary kidney tumors and metastatic lesions. SBRT’s ability to deliver ablative doses to the tumor contributes to effective local tumor control.
Technical Advances
– Advancements in radiation therapy techniques, such as image-guided radiation therapy (IGRT) and intensity-modulated radiation therapy (IMRT) & Volumetric Modulated Arc Therapy (VMAT) & Motion Management Systems (RPM) & Respiratory Gating systems allow for precise targeting of tumors while sparing adjacent normal tissues. This is particularly important in kidney cancer where minimizing damage to healthy kidney tissue is crucial. While surgery remains the primary treatment for localized kidney cancer, radiation therapy can play a valuable role in specific situations, such as adjuvant treatment for high-risk cases, palliation of symptoms in advanced disease, and in combination with other therapies. Ongoing research continues to explore the optimal integration of radiation therapy into the multidisciplinary management of kidney cancers.
What to expect during radiation therapy for kidney cancer?
The exact course of radiation therapy will vary depending on the individual’s specific case. However, in general, patients can expect:
- Consultation: A doctor will discuss the benefits and risks of radiation therapy and develop a personalized treatment plan.
- Before treatment begins, patients will undergo a simulation session to ensure precise targeting of the radiation beams.
- Treatment sessions: Each session typically lasts for 15-30 minutes and is administered five days a week for several weeks.
- Follow-up care: Patients will be monitored regularly after treatment to check for any side effects and assess the effectiveness of the treatment.
Benefits of radiation therapy for kidney cancer
- Non-invasive: Unlike surgery, radiation therapy does not require any incisions or hospitalization.
- Targeted treatment: Radiation can be precisely focused on the tumor, minimizing damage to surrounding healthy tissues.
- Effective pain relief: Radiation can significantly reduce pain and other symptoms associated with advanced kidney cancer.
- Potential for cure: In some cases, radiation therapy can be curative, especially for small, localized tumors.
Side effects of radiation therapy for kidney cancer
As with any medical treatment, radiation therapy can cause some side effects. These can vary depending on the type and dose of radiation received but may include:
- Fatigue
- Nausea and vomiting
- Skin irritation
- Hair loss
- Loss of appetite
In most cases, these side effects are mild and temporary and can be managed with medication and supportive care.
Radiation therapy is a valuable tool in managing kidney cancer. It can be used as a primary treatment for individuals who cannot undergo surgery, to alleviate symptoms caused by advanced cancer, or to prevent the recurrence of the disease. While there are potential side effects, they are often manageable and outweighed by the benefits of treatment.
Consult our expert, Dr. Sandeep De, Sr. Consultant Radiation Oncology, Apollo Cancer Centres, Navi Mumbai for all queries and consultation for radiation therapy for any form of cancer.
Call 022 6280 6280 for an appointment.
- October 22, 2024
World Stroke Day: Raising Awareness and Saving Lives
- October 22, 2024
Robotic Surgery in Gynecology: A Revolution in Women’s Health
- October 22, 2024
Robotic Surgery in General Surgery
- October 22, 2024
Pediatric Neurosurgery: Complexities of Brain Tumors in Children
- October 22, 2024
LGBTQ+ and Cancer: Challenges and Support
- Bone Marrow Transplant3
- Cardiac sciences44
- Child Care7
- Clinical Excellence33
- Cosmetology2
- COVID-199
- Diseases4
- Emergency8
- Emergency10
- Endocrinology1
- ENT5
- Fetal Medicine1
- Gastroenterology6
- General Medicine9
- General Surgery3
- Genomic Medicine2
- Gynecology1
- Health14
- Hematology2
- Kidney Transplant5
- Kidney Transplant2
- Liver Transplant6
- Neonatology1
- Nephrology2
- Nephrology & transplant1
- Nephrology & Urology4
- Neurosciences1
- Neurosciences20
- Nutrition/Diet1
- Obstetrics & Gynecology9
- Obstetrics & Gynecology4
- Oncology92
- Oncology3
- Ophthalmology1
- Orthopedic13
- Patient Speak1
- Pediatric Surgery3
- physiotherapy2
- Psychologist2
- Pulmonology1
- Rheumatology1
- Robotic Suregry1
- Robotic Surgery11
- Spine1
- Uncategorized111
- Women Care5
